Home » New Initiatives Set to Enhance Medical Support for Black Communities
New Initiatives Set to Enhance Medical Support for Black Communities
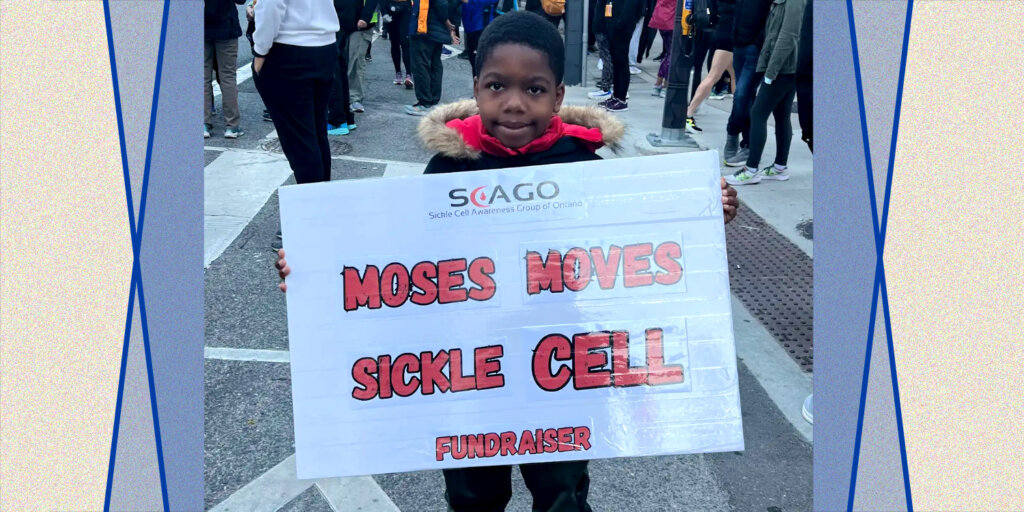
The interplay of trust and care significantly influences healthcare experiences, particularly for marginalized communities. This dynamic is exemplified in the case of six-year-old Moses, who was hospitalized at Toronto's SickKids for a vaso-occlusive crisis due to sickle cell disease, a condition he learned about shortly after birth. His mother, D. Ramsay, faced numerous challenges while seeking care, including a lack of knowledge about sickle cell disease among medical professionals. Her experiences highlight systemic barriers, particularly for individuals from African, Caribbean, and Black (ACB) communities, which constitute a significant portion of sickle cell patients in Canada.
Moses's hospitalization also drew attention to broader health disparities faced by ACB populations. Systemic racism and discrimination across areas like education and housing undermine their well-being and access to adequate healthcare. Black Canadians suffer from healthcare inequities, including higher rates of diabetes compared to their white counterparts. This was underscored by Jacqueline Getfield, project manager at University Health Network’s Caribbean African Regenerative Medicine (CARM) initiative, which aims to bridge the gap between ACB individuals and advancements in regenerative medicine.
CARM is working towards fostering care and trust in healthcare systems, essential in addressing chronic health issues prevalent in ACB communities, such as diabetes and sickle cell disease. Regenerative medicine, which encompasses innovative approaches like gene therapy and stem-cell transplants, holds the potential to revolutionize treatment options for such conditions. Through collaborations among researchers, medical professionals, and community members, CARM aims to enhance medical support for Black communities and enable informed health decisions.
Promising new treatments in regenerative medicine include gene therapy, which has seen recent approvals in Canada. This therapy could enable sickle cell patients to utilize their own genetically modified stem cells to cure the disease. However, access remains limited due to the high costs associated with such treatments, presenting barriers for families in need of assistance like the Ramsays, who have taken proactive measures, such as saving their newborn son’s umbilical cord blood for future use.
Efforts to improve healthcare access for the ACB community also involve increasing participation in national stem cell registries to address the notable lack of Black donors. Organizations like Donor Drive 4 Dorothy (DD4D) promote awareness and participation in these registries, emphasizing the critical need for diverse donor options. While the overall donor pool in Canada is lacking in diversity, engaging young Black Canadians in these initiatives can significantly enhance matching success rates.
Dr. Carl James, a sociologist and co-lead investigator in CARM, emphasizes the historical reluctance among ACB community members to engage with healthcare professionals due to past experiences of racism and mistrust. This sentiment illustrates the importance of diversifying healthcare providers to foster trusting relationships. Getfield highlights the need for a comprehensive understanding of the diverse values and backgrounds within the ACB community to create an inclusive healthcare system.
CARM aims to raise awareness about regenerative medicine and integrate it into conversations within Black communities. Getfield stresses that early education about health sciences can inspire future generations to pursue careers in this field, ultimately leading to more robust solutions for chronic health issues faced by ACB individuals. By establishing trust and increasing representation in healthcare, initiatives like CARM seek not only to improve individual health outcomes but also to cultivate a healthier community as a whole.
MaRS Discovery District
https://www.marsdd.com/
MaRS is the world's largest urban innovation hub in Toronto that supports startups in the health, cleantech, fintech, and enterprise sectors. When MaRS opened in 2005 this concept of urban innovation was an untested theory. Today, it’s reshaping cities around the world. MaRS has been at the forefront of a wave of change that extends from Melbourne to Amsterdam and runs through San Francisco, London, Medellín, Los Angeles, Paris and New York. These global cities are now striving to create what we have in Toronto: a dense innovation district that co-locates universities, startups, corporates and investors. In this increasingly competitive landscape, scale matters more than ever – the best talent is attracted to the brightest innovation hotspots.